Services
Anti-Reflux Surgery
LAPAROSCOPIC SURGERY FOR “HEART BURN”
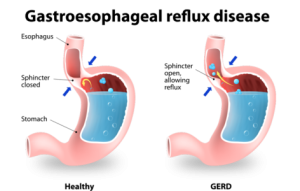
What is Gastroesophageal Reflux Disease (GERD)?
- Although “heartburn” is often used to describe a variety of digestive problems, in medical terms, it is actually a symptom of gastroesophageal reflux disease.
- In this condition, stomach acids reflux or “back up” from the stomach into the esophagus.
- Heartburn is described as a harsh, burning sensation in the area in between your ribs or just below your neck. The feeling may radiate through the chest and into the throat and neck.
- Other symptoms may also include vomiting, difficulty swallowing and chronic coughing or wheezing.
What Causes GERD?
- When you eat, food travels from your mouth to your stomach through a tube called the esophagus. At the lower end of the esophagus is a small ring of muscle called the lower esophageal sphincter (LES). The LES acts like a one-way valve, allowing food to pass through into the stomach.
- Normally, the LES closes immediately after swallowing to prevent back-up of stomach juices, which have a high acid content, into the esophagus.
- GERD occurs when the LES does not function properly allowing acid to flow back and burn the lower esophagus. This irritates and inflames the esophagus, causing heartburn and eventually may damage the esophagus.
What Contribute to GERD?
- Some people are born with a naturally weak sphincter (LES). For others, however, fatty and spicy foods, certain types of medication, tight clothing, smoking, drinking alcohol, vigorous exercise or changes in body position (bending over or lying down) may cause the LES to relax, causing reflux.
- A hiatal hernia (a common term for GERD) may be present in many patients who suffer from GERD, but may not cause symptoms of heartburn.
How to Diagnosis GERD?
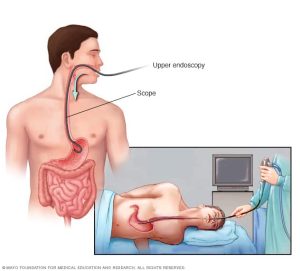
Diagnosis of GERD generally based on a history of your signs and symptoms and a physical examination.
To confirm a diagnosis of GERD, or to check for complications, Dr.Sharma might recommend:
- Upper endoscopy.
- Ambulatory acid (pH) probe test.
- X-ray of the upper digestive system.
- Esophageal manometry. This is typically done in people who have trouble swallowing.
How is GERD Treated ?
Treatment is generally in three progressive steps:
Lifestyle and Dietary Changes
Dietary and lifestyle changes are the first step in treating GERD. Certain foods make the reflux worse. Suggestions to help relieve symptoms include:
- Lose weight if you are overweight — of all of the lifestyle changes you can make, this one is the most effective.
- Avoid foods that increase the level of acid in your stomach, including caffeinated beverages.
- Avoid foods that decrease the pressure in the lower esophagus, such as fatty foods, alcohol and peppermint.
- Avoid foods that affect peristalsis (the muscle movements in your digestive tract), such as coffee, alcohol and acidic liquids.
- Avoid foods that slow gastric emptying, including fatty foods.
- Avoid large meals.
- Quit smoking.
- Do not lie down immediately after a meal.
- Elevate the level of your head when you lie down.
Medication
If lifestyle and dietary changes do not work, Dr. Sharma may prescribe certain medications. There are two categories of medicines for reflux. One decreases the level of acid in your stomach, and one increases the level of motility (movement) in the upper gastrointestinal tract.
Surgery for GERD
If your symptoms did not improve with lifestyle changes or drug therapy, you may be a candidate for surgery. Some patients prefer a surgical approach as an alternative to a lifetime of taking medications. The goal of surgery for reflux disease is to strengthen the anti-reflux barrier.During a procedure known as a Nissen fundoplication, Dr. Sharma wraps the upper part of your stomach around the lower esophagus. This enhances the anti-reflux barrier and can provide permanent relief from reflux. Dr. Shrama perform this surgery laparoscopically, which means a less invasive procedure with a shorter recovery time.
Are you a candidate for the Laparoscopic Surgery?
Although laparoscopic anti-reflux surgery has many benefits, it may not be appropriate for some patients. Obtain a thorough medical evaluation by a surgeon qualified in laparoscopic anti-reflux surgery to find out if the surgery is appropriate for you.
How is Laparoscopic Surgery performed?

Laparoscopic anti-reflux surgery (commonly referred to as Laparoscopic Nissen Fundoplication) involves reinforcing the “valve” between the esophagus and the stomach by wrapping the upper portion of the stomach around the lowest portion of the esophagus – much the way a bun wraps around a hot dog.
- In a laparoscopic procedure, surgeons use small incisions (0.5 to 1 cm) to enter the abdomen through cannulas (narrow tube-like instruments). The laparoscope, which is connected to a tiny video camera, is inserted through the small incision, giving Dr.Sharma magnified view of your internal organs on a television screen.
- The entire operation is performed “inside” after the abdomen is expanded by inflating gas into it.
What happens if the operation cannot be performed or completed by the Laparoscopic Method?
In a small number of patients the laparoscopic method is not feasible because of the inability to visualize or handle the organs effectively. Factors that may increase the possibility of converting to the “open” procedure may include obesity, a history of prior abdominal surgery causing dense scar tissue, or bleeding problems during the operation. The decision to perform the open procedure is a judgment decision made by Dr. Sharma either before or during the actual operation. When Dr Sharma feels that it is safest to convert the laparoscopic procedure to an open one, this is not a complication, but rather sound surgical judgment. The decision to convert to an open procedure is strictly based on patient safety.
What should I expect after surgery?
- Patients are encouraged to engage in light activity while at home after surgery.
- Post operative pain is generally mild although some patients may require prescription pain medication.
- Anti-reflux medication is usually not required after surgery.
- Some surgeons modify patients diet after surgery beginning with liquids followed by gradual advance to solid foods.
- You will probably be able to get back to your normal activities within a short amount of time. These activities include showering, driving, walking upstairs, lifting, working and engaging in sexual intercourse.
- Take follow up appointment within 2 weeks after your operation.
What Are the side effects of this procedure?
Studies have shown that the vast majority of patients who undergo the procedure are either symptom-free or have significant improvement in their GERD symptoms.
Long-term side effects to this procedure are generally uncommon.
- Some patients develop temporary difficulty swallowing immediately after the operation. This usually resolves within one to three months after surgery.
- Occasionally, patients may require a procedure to stretch the esophagus (endoscopic dilation) or rarely re-operation.
- The ability to belch and or vomit may be limited following this procedure. Some patients report stomach bloating.
- Rarely, some patients report no improvement in their symptoms.
When to Call
Be sure to call/consult, if you develop any of the following:
- Persistent fever over 101 degrees F (39 C)
- Bleeding
- Increasing abdominal swelling
- Pain that is not relieved by your medications
- Persistent nausea or vomiting
- Chills
- Persistent cough or shortness of breath
- Purulent drainage (pus) from any incision
- Redness surrounding any of your incisions that is worsening or getting bigger
- You are unable to eat or drink liquids

